Considering having your beloved companion anesthetized can create many different worries and second thoughts in most people. This is very understandable. Many people may have heard a story of someone’s pet dying while under anesthesia for a routine procedure. Many of those cases happened a long time ago, thankfully, and modern anesthetic techniques have drastically improved patient safety.
At SJVC, we are very proud of our anesthetic safety record which we have earned through careful consideration of every patient. Our team is diligent, uses constant monitoring, and performs rapid intervention when needed.
The most common reasons a pet needs to undergo anesthesia include:
- -Dental Hygiene Procedure
- -Sterilization (spay or neuter)
- -Mass removal or tissue biopsy
- -Trauma (orthopedic fracture, laceration, etc)
- -Exploratory abdominal surgery
- -Other varieties of exploratory procedures and treatments
Anesthesia is an amazingly wonderful tool that allows us to perform life-saving and health improving procedures on a daily basis. Anesthesia can be broken down into 2 main categories: 1) Sedation and 2) General Anesthesia. These are both performed with the animal’s health, comfort and safety as our primary consideration.
Sedation is a very common practice to allow us to investigate and treat an animal more invasively than they would tolerate while awake. This is typically achieved by giving the animal either an intravenous or intramuscular injection of a combination of anesthetic agents that can be reversed after the procedure is complete. The animal is asleep and feels no pain but is still able to control their airway and blink.
General Anesthesia is required for more invasive, more stimulating or longer procedures. This involves 3 phases of anesthetic agents being administered to slowly calm the animal, maintain good cardiovascular function, provide pain control, and keep them asleep very safely for as long as we need to complete their procedure.
For general anesthesia we first perform a thorough physical exam on every patient.

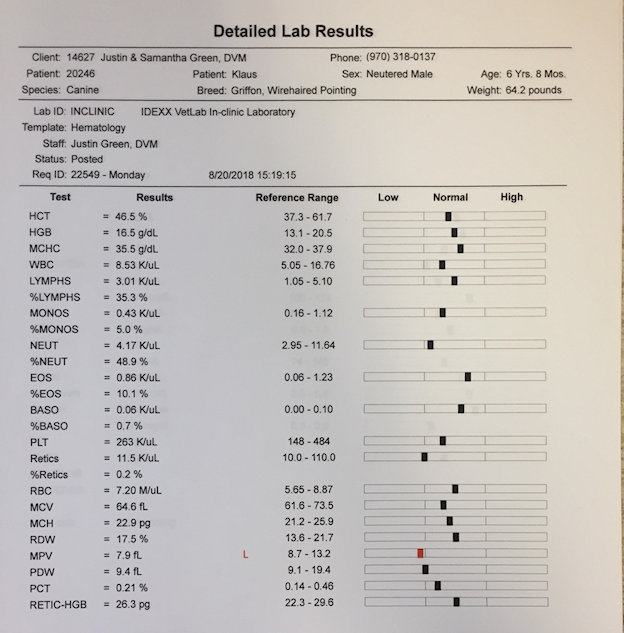
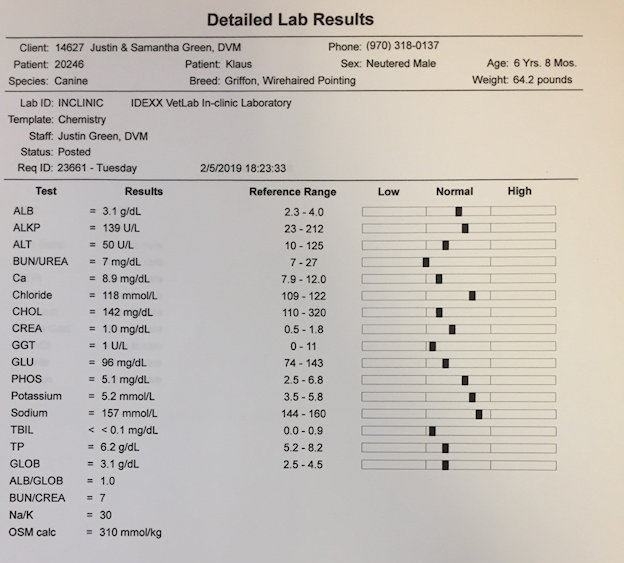
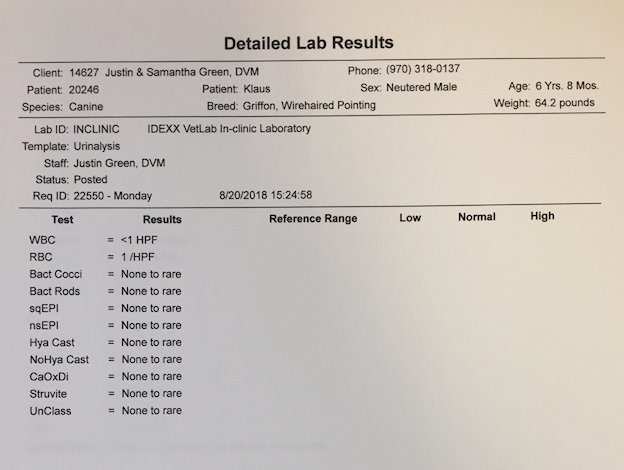
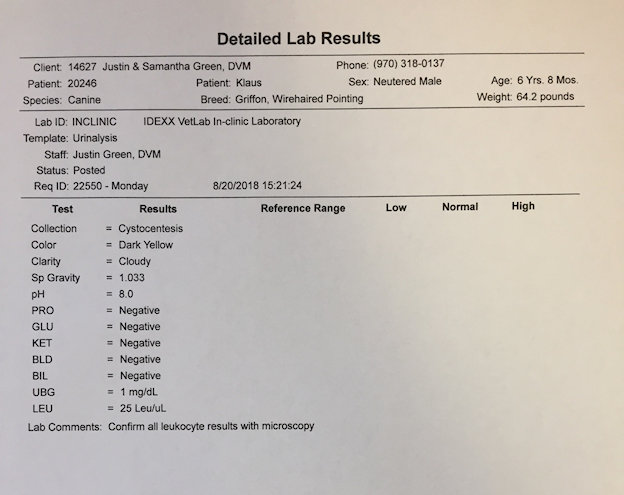
Second we analyze pre-anesthetic lab work including a complete blood cell count (CBC), serum chemistry panel, and urinalysis to ensure all of your pet’s organs are functioning normally.
If the patient’s physical exam and laboratory test results demonstrate a healthy animal, we proceed with the 1st phase of anesthesia which is typically a subcutaneous injection of a combination of 3 drugs intended to sedate, provide pain control and regulate cardiovascular function. Once this takes full effect (usually 20-30 minutes) the patient receives an intravenous catheter and is given supplemental oxygen.


This allows the 2nd phase of anesthesia where the patient is anesthetized with an IV injection of typically 1 or 2 anesthetic agents. Once they are sound asleep, a breathing tube is placed to allow us to deliver oxygen and an anesthetic gas. This is the 3rd phase of anesthesia and is used to keep the patient asleep for the duration of the procedure.


Anesthetic support and monitoring are critical to the success of the anesthetic experience. This vigilance is the primary reason anesthesia is safer today than ever before in history.
A typical anesthetized patient receives IV fluids throughout the entire procedure to support optimal blood pressure and maintain ideal tissue perfusion.
Each patient also has eye lubricant applied to keep their eyes from drying out and is kept comfortable and warm with a warm water blanket, hot towels, warm rice socks and an IV fluid warmer.

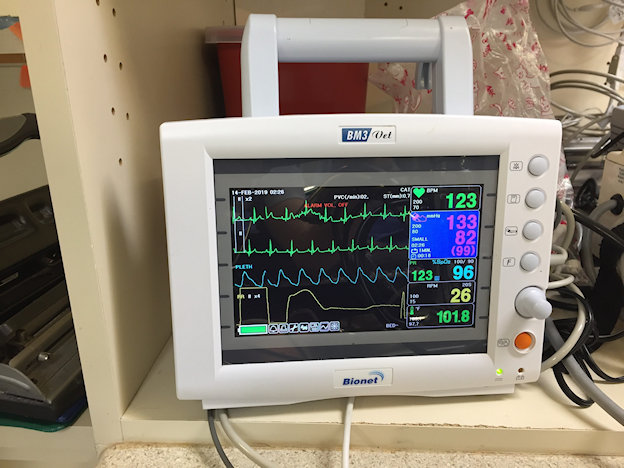
Throughout the procedure we constantly monitor several aspects of the patient’s cardiovascular and pulmonary function. This typically includes ECG, Blood Pressure, Pulse-ox (blood oxygen saturation), Temperature, Respiratory Rate, CO2 expiration, Inhaled Oxygen level and anesthetic gas level.
If a procedure is expected to be painful we provide additional pain control measures whenever possible to lower the amount of anesthetic required. This typically would include topical anesthesia (eyes), local anesthesia (laceration), regional nerve blocks (dental/ oral surgery), epidural anesthesia (orthopedic surgeries), and intra-operative pain medication such as anti-inflammatories, lidocaine drips, opioid drips and pain patches.

Anesthesia is a serious endeavor and should be treated as such. However, a well-planned drug protocol, pre-anesthetic health assessment and diligent monitoring help to make anesthesia very safe. Avoiding a life improving procedure out of fear of anesthesia is not necessary. If you have any concerns about your pet’s safety during an upcoming anesthesia, our well trained staff is happy to answer any questions and listen to any concerns to ensure you are completely comfortable before proceeding. Our entire purpose is to improve the life of your companion, together with you.
Happy Trails!!



 Life has a way of surprising us at times. A random meeting of a veterinarian and an owner with an emergency on Christmas Day which led to wonderful reunion. The veterinarian, Dr. Cotton and her family, spend their vacation time on Cat Island, a remote out island in the Bahamas. This island has a local population of island dogs called Potcakes. These dogs are often born in unusual places as many roam wild without owners. This particular dog had been born in the local dump and she was adopted by a man from Colorado who happened to spend time on this island. The dog, Blondie, and owner spent time near Dr. Cotton's home on the island and many times wandered on her porch and into her house to say hi. The owner and his dog became friends with Dr. Cotton and she and her family would often see them fishing on the North shore in the evenings. Blondie's owner passed away and she was adopted by the owner's sister several years ago.
Life has a way of surprising us at times. A random meeting of a veterinarian and an owner with an emergency on Christmas Day which led to wonderful reunion. The veterinarian, Dr. Cotton and her family, spend their vacation time on Cat Island, a remote out island in the Bahamas. This island has a local population of island dogs called Potcakes. These dogs are often born in unusual places as many roam wild without owners. This particular dog had been born in the local dump and she was adopted by a man from Colorado who happened to spend time on this island. The dog, Blondie, and owner spent time near Dr. Cotton's home on the island and many times wandered on her porch and into her house to say hi. The owner and his dog became friends with Dr. Cotton and she and her family would often see them fishing on the North shore in the evenings. Blondie's owner passed away and she was adopted by the owner's sister several years ago.